
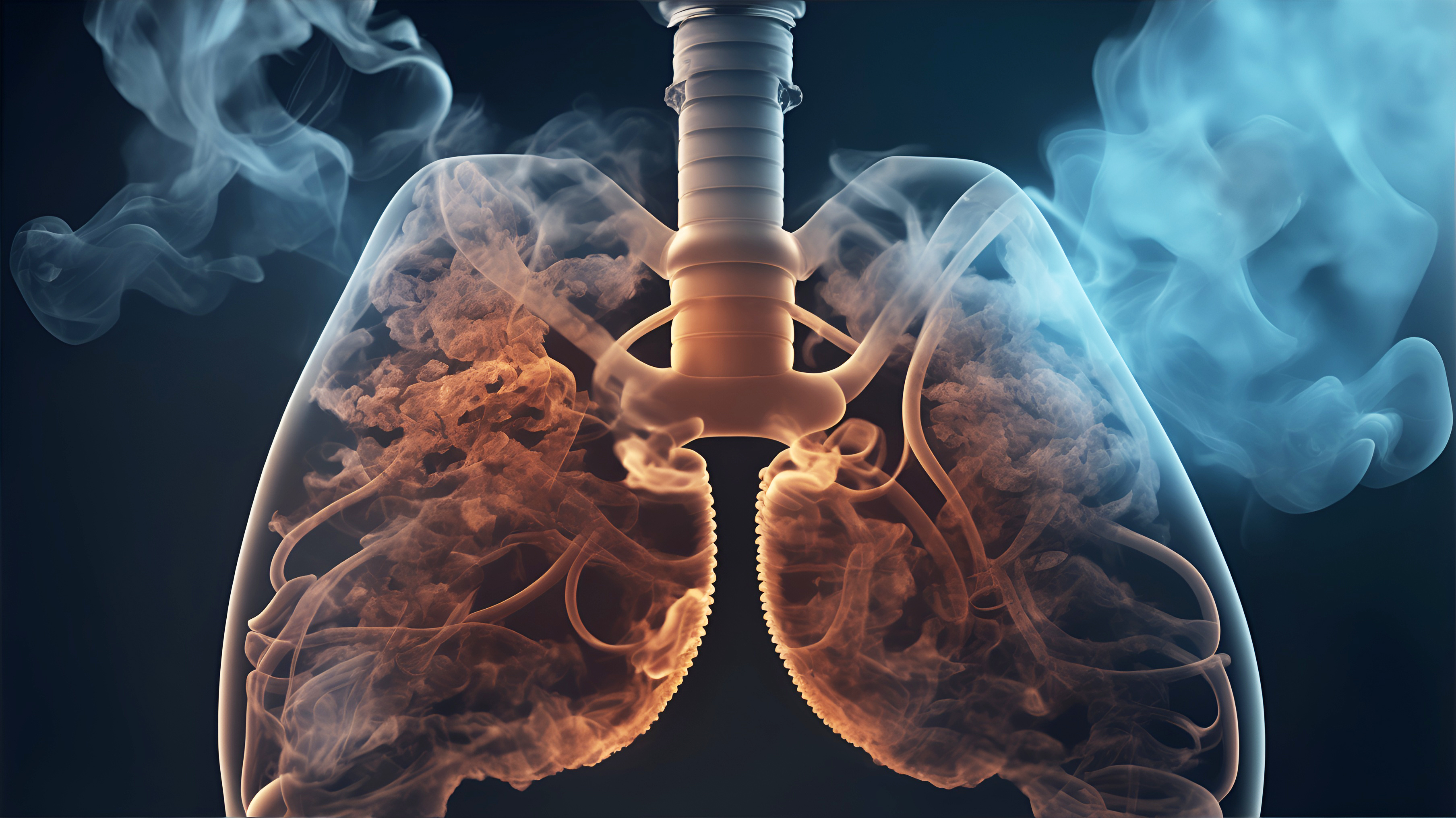
Alveolar Macrophages Drive Smoke-Induced Lung Damage
Discover breakthrough insights into COPD: Our co-founder Kevin Baßler is co-author of a pivotal study that reveals how smoking triggers certain immune cells to trigger lung inflammation. This research opens up new avenues for targeted COPD therapies, with inhibition of IRAK4 kinase yielding promising results. Let's dive in!
COPD and Smoking-Induced Lung Inflammation
Chronic obstructive pulmonary disease (COPD) is a progressive inflammatory disorder with significant global impact, characterized by chronic lung inflammation, irreversible airflow limitation, and structural changes in the lung such as emphysema. Cigarette smoking is the major risk factor for COPD, inducing tissue injury through both oxidative stress and inflammation. Despite the recognized role of inflammation in COPD pathogenesis, the precise cellular and molecular basis of smoking-induced lung inflammation remains obscure.
Insights from Single-Cell Genomics
The application of single-cell RNA-sequencing (scRNA-seq) in murine smoke exposure models has provided unparalleled detail into the cellular landscape of smoking-induced lung inflammation. This cutting-edge approach allows for the dissection of complex cell populations and their interplay, with a focus on the role of alveolar macrophages (AM) and neutrophils in the alveolar space.
Unraveling the Inflammatory Loop
The study's integrative analysis across acute, sub-chronic, and chronic stages of smoke exposure has unveiled a self-amplifying inflammatory loop driven by the following components:
Molecularly diverse neutrophil subsets that serve as key inflammatory amplifiers.
Monocyte-derived alveolar macrophages (MoAM) that are pro-inflammatory and critical in pathological tissue remodeling, a stark contrast to tissue-resident AM.
Translational Relevance to Human COPD
The findings extend beyond the murine models, with the identification of pro-inflammatory MoAM orthologs in human emphysematous COPD patients. This correlation underscores the practical significance of the research and its potential to inform future therapeutic interventions.
Potential Therapeutic Target: IRAK4 Kinase Inhibition
A promising therapeutic avenue emerges with the evidence that pharmacological inhibition of IRAK4 kinase can diminish the recruitment of both neutrophils and MoAM, thereby reducing inflammation in the lungs of smoke-exposed mice. This points to a new potential strategy for managing inflammation in smoking-related lung disease.
The comprehensive insights from this study not only deepen our understanding of COPD pathogenesis but also pave the way for the development of innovative treatments targeting specific components of the inflammatory process induced by smoking.
Results
#1 Impact of Acute Smoke Exposure on Immune Cell Dynamics
Acute smoke exposure for four days instigated a marked shift in the pulmonary immune cell landscape. Through single-cell RNA sequencing of cells from bronchoalveolar lavage fluid (BALF) and lung tissue, researchers observed a drastic change in cell composition. Neutrophils surged into the airspace, composing 72% of BALF cells in smoke-exposed mice, whereas they were non-existent in controls. Additionally, a novel subset of Itgam+ alveolar macrophages (AM) emerged exclusively in smoke-exposed animals, contributing to a 2.4-fold increase in macrophages within BALF. These results suggest that acute smoke exposure ignites neutrophilic inflammation and introduces a unique AM subset, reshaping the immune environment in the lung.
#2 Heterogeneity and Functionality of Neutrophils Post-Smoke Exposure
The study delved into the transcriptomes of neutrophils and AM, revealing that acute smoke exposure stimulated a diverse range of neutrophil subclusters with distinct functionalities. One subset, in particular, was identified as a key player in the inflammatory milieu, expressing high levels of pro-inflammatory chemokines and cytokines. Another subset indicated signs of aging or senescence, while others appeared to be newly recruited with active migration and chemotaxis markers. This diversity underscores the pivotal role of neutrophils as early regulators of the inflammatory response to smoke.
#3 Classical Monocytes Contribute to AM Pool During Inflammation
A closer examination of the immune cell population hinted at a pathway from classical monocytes (CMo) to interstitial macrophages (IM) and monocyte-derived alveolar macrophages (MoAM). Trajectory analysis supported this progression, with CMo transitioning through an intermediate state before differentiating into MoAM. This differentiation seemed to be regulated transcriptionally in a niche-specific manner, indicating that CMo recruitment and conversion play a significant role in the inflammatory response to smoke exposure.
#4 Role of MoAM in Smoke-Induced Lung Inflammation
MoAM displayed a distinct gene expression profile, strongly associated with tissue remodeling and pro-inflammatory pathways. Their expression of chemokines implicated in the recruitment of neutrophils, T cells, and MoAM suggests a central function in perpetuating inflammation. Furthermore, the presence of MoAM was linked with a tissue remodeling signature, implicating them in pathological changes within the lung, including emphysema.
#5 Chronic Smoke Exposure and MoAM Increase
Chronic smoke exposure led to a persistent rise in MoAM, altering the AM pool to favor a more inflammatory and tissue remodeling phenotype. This shift was evidenced by an increased proportion of MoAM over time, which correlated with a progression to emphysema and impaired lung function in murine models. Histological assessments confirmed the presence of pulmonary emphysema, supporting the notion that MoAM are instrumental in chronic lung inflammation and tissue remodeling.
#6 Human Relevance: MoAM Orthologs in Emphysema Patients
The study extended its relevance to human COPD by identifying an increase in MoAM orthologs within emphysematous patients. These human MoAM exhibited a gene signature similar to murine MoAM, enriched for tissue remodeling and pro-inflammatory markers. This finding implies that the mechanisms unraveled in mice may be translatable to human emphysema, providing a potential biomarker for the disease.
#7 Anti-Inflammatory Effects of IRAK4 Inhibitor Treatment
Intervention with an IRAK4 inhibitor demonstrated significant anti-inflammatory effects, reducing the levels of pro-inflammatory cytokines and chemokines in BALF. This treatment also led to a reduction in MoAM and neutrophil recruitment, including a notable depletion of a specific pro-inflammatory neutrophil subset. These results highlight the potential of targeting inflammatory signaling pathways as a therapeutic strategy for smoking-induced lung inflammation.

Discussion
The comprehensive study concludes with a thorough discussion, emphasizing the significant impact of cigarette smoking as the single most preventable cause of illness and death and its status as a leading risk factor for COPD. Through the use of single-cell RNA sequencing, this study has illuminated the complexities of immune cell dynamics that contribute to smoking-induced lung inflammation and the progression to chronic COPD and emphysema.
The researchers discovered a previously unappreciated diversity in cell populations and molecular responses during the progression of smoke-induced lung inflammation. Notably, the study revealed the progressive increase of monocyte-derived alveolar macrophages (MoAM) and their distinct transcriptional identity from resident AM. These MoAM are implicated as central drivers of lung inflammation, with their accumulation associated with the development of emphysema. The study's translational relevance is further strengthened by the finding that human orthologs of MoAM are also increased in emphysematous COPD patients, underscoring the potential of translational approaches to uncover cellular alterations in human disease.
Monocytes' Dual Fate and Emphysema Development
The discussion highlights that the molecular profile of MoAM, including markers associated with tissue remodeling and emphysema, suggests their direct involvement in disease pathogenesis. The study contrasts with previous research by suggesting a dual fate for classical monocytes, which may differentiate into both interstitial macrophages and MoAM in response to cigarette smoke. This dual pathway challenges established concepts and suggests that cigarette smoke exposure may trigger an increased differentiation of monocytes into MoAM, which, along with proliferating resident AM, contributes to macrophage increases and tissue damage.
The study also underscores the importance of MoAM's pro-inflammatory profile, a finding consistent with previous literature on acute inflammatory conditions. It further suggests that chronic smoking establishes a self-amplifying inflammatory loop, with MoAM as key inflammatory regulators, leading to chronic pulmonary inflammation and emphysema. Pro-inflammatory mediators strongly expressed by MoAM, including CCL2 and CCL7, have been linked to COPD and are implicated in the recruitment of inflammatory cells to the lungs.
Therapeutic Potential of IRAK4 Inhibition
The researchers also discuss the potential therapeutic implications of their findings. They demonstrate that pharmacological inhibition of IRAK4, a kinase involved in TLR and IL-1 signaling, can significantly reduce inflammatory burden and recruitment of pro-inflammatory cells. The study concludes with the following statement, encapsulating the significance of the findings:
 Our study indicates that pharmacological IRAK4 inhibition disrupts the smoke-induced self-amplifying inflammatory loop which makes it also an attractive therapeutic concept for COPD.
Our study indicates that pharmacological IRAK4 inhibition disrupts the smoke-induced self-amplifying inflammatory loop which makes it also an attractive therapeutic concept for COPD.
In summary, the study provides new insights into the mechanisms underlying smoke-induced COPD and identifies potential therapeutic targets. It lays the groundwork for future research into COPD subtypes and tailored treatment strategies, with an emphasis on the importance of targeting MoAM, neutrophil subsets, and their inflammatory signaling pathways in clinical trials.
We invite you to delve deeper into the methods and results and take a look at the original study!